Read More »
Read More »
Read More »
Read More »
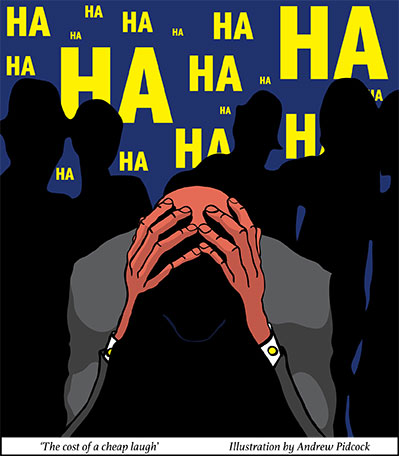
In the first article we covered some of the basic concepts in understanding and preventing workplace bullying. We outlined bullying definitions, legal considerations, the assessment process, and issues of potential bias in the assessment process. We will now consider the effective management strategies required to support key stakeholders, particularly the injured worker. We will be discussing this in context of the roles and perspectives of the various stakeholders involved in a claim.
Managing the claim
If a workers compensation psychological injury claim is to be managed well a thorough unbiased assessment needs to be undertaken combining the inputs and perspectives of the various stakeholders. This is essential because the information obtained will determine strategies that are incorporated to treat the injured worker, to address the issues contributing to the psychological claim, as well as to determine the time frames and priorities of the various interventions. The claim as discussed in the first article, will be investigated by an independent assessor, and the worker examined by an independent doctor. An injury management plan is put together by the insurer outlining stakeholders (such as the GP, the employer, the worker, the insurer and the psychologist/psychiatrist of their obligations and roles in the management and support of the injured worker.
Some of the important information includes:
The workers current mental health and prognosis
There are a number of factors that influence how a worker will have responded to bullying, including the intensity of bullying, the frequency, the nature of the bullying and the time frames in which it took place. Sometimes trauma symptoms can result. Also to be considered is the culture of the organisation. Was bullying supported or were steps taken to prevent or minimise the employer’s behaviour. The role of the worker in the bullying and subsequent reactions must also be considered when strategies are being planned to treat the workers resulting “psychological injuries” and in ensuring that the underlying issues are addressed that led to the claim. Consideration must be given to the general resilience of the worker and what strategies they were able to call upon to manage the past situations and to determine their reaction.
It is important that the professionals assessing and /or supporting the bullied worker (i.e. that the “independent medical examination”) looks at these issues and gives feedback in their initial report, and the treating psychologist or psychiatrist who is involved considers these issues and gives appropriate feedback to the stakeholders, particularly the NTD.
The psychologist or psychiatrist managing the psychologically injured worker needs to take a thorough history of not only the bullying but of other aspects of the workers personality so that the approach and treatment priorities can be given that will be most effective for that individual. Although there are specific evidence based treatments that should be applied, the way these are presented needs to be tailored to the individual.
The type of problems bullied injured workers may experience.
Assuming the employee was not experiencing any significant other mental health issue over the time the bullying took place and that the employer was generally coping with life, it is probable that the psychological consequences of the bullying will lead changes in the three key areas of psychological functioning - thinking, feeling and motivation.
Stress responses are on a continuum ranging from arousal (we need a certain amount of stress / arousal to just get out of bed in the morning) to a full-blown panic attack (where there are marked physiological and psychological changes that make normal functioning impossible). Physiological responses to stress include tense muscles, shallower breathing, an increase in heart rate, restlessness, dilated pupils and sweaty palms. It may include nausea vomiting, diarrhoea, loss of appetite and significant sleep disturbances. Psychological cognitive responses include rapid thinking, poor concentration, difficulty in decision making, poor judgements when thinking, intrusive thoughts, “I can’t get the thoughts out of my mind”, catastrophic thinking and only seeing the worse possible scenarios, and cognitive rigidity where you can only see a very limited range of options. The feeling (affective) responses may include agitation, irritability, a labile mood where the mood is all over the place, depression, fear and dread about returning to the place where the stress was induced. Motivation and energy level changes also occur and a range of agitation and inability to relax as well as extreme fatigue, and exhaustion where everything is overwhelming.
Prolonged stress often precipitated by extended periods of bullying can and usually does eventually lead to clinical depression. Many of the symptoms described may eventually become so severe that there is major impairment in everyday functioning and capacity to cope with the demands of life. Some of the key diagnostic criteria for major depressive disorder include:
It is not unusual for health professionals to first see a once normally high functioning resourceful and normally resilient patient present to the consulting room after months with extreme depression of major depression after years of trying to manage the situation at work by themselves and only after years of dysfunctional relationships and dynamics do they finally “crack”
There are some unfortunate workers who have experienced threats of violence against them or who have been physically assaulted. In these situations or similar situations where they have been exposed to a critical incident of threatened harm or have witnessed injury or death, a trauma response is probable, and symptoms of a post-traumatic stress disorder (PTSD) may also follow. The diagnostic criteria for PTSD includes:
Treating
the Injured Worker
A psychologist tends to provide precise and gentle feedback to the worker including an adequate explanation of the strategies and therapies they need to incorporate into their lives to get better. Communication and management is essential for commitment to therapy and in moving towards a graded plan for returning to work.
Strategies and treatments that are most effective include
The injured worker needs to be supported and treated for the psychological injury they sustained as a result of the bullying experiences, as well as developing on reducing and managing their “symptoms”. Therapy should encompass strategies for minimising the chances for such reactions to occur again. Some of the strategies may include:
Dealing with what happened at Work?
The emphasis on management of bullying needs to be spread fairly - and will include looking at what happened at work and what can be done at work to support the injured worker in the future. Consideration needs to be given to:
The injured worker will only be able to return to work when the treating doctor certifies him/her as fit to do so. In most bullying claims the injured worker will be getting treatment from a psychologist, and / or a psychiatrist and it will be essential that their input is gathered from the NTD.
In some situations it is not appropriate for the bullied worker to go back to work site at all, and they may need to change employers or occupations. This is most likely to occur when the bullying was severe, frequent and occurred over a prolonged period of time, when efforts were made by the worker to get support to stop the bullying resulting in them being ignored or dismissed by an employer, and in situations where physical assault actually occurred. In most of these cases the injured worker is likely to have a significant psychological injury where there is substantial loss of confidence, self-esteem, concentration and focus. Although the severity of the initial symptoms may have eased the injured worker may still not have the capacity to work at the same level and at the same pace (dealing with and processing information) the way they did before the injury. In these situations a work trial is advisable after a vocational assessment is undertaken.
The work trial is usually performed with fewer numbers of hours than pre-injury and with lower workload demands. The hours and duties can be increased progressively according to tolerances and a person’s overall health standing. At some point a decision will need to be made as to whether the injured worker can and should return to the pre-injury work site and employer. The decision needs to be made using all the information and should include:
There are other situations where the worker can immediately return to their pre-injury work site, and may be able to return immediately to their old role. This may be appropriate if the bullying was not for a prolonged period, the worker’s injury is relatively mild, if the situation has changed at the work site in terms of the bully or bullies having been spoken to, and or if they are no longer working in the section of the workers pre-injury workplace.
Workplace mediation is sometimes an extremely helpful and a necessary strategy to help parties with conflicting views and issues to better understand each other and to develop strategies for managing their differences. There are a number of different mediation models, however the ones that are most effective allow the mediator to firstly speak privately to the various parties involved, to outline their needs, fears and to allow them to ventilate their concerns before they meet with the other parties. A good outcome from mediation will include better understanding and acceptance of each party’s points of view, a diffusing of anger and fear, and a specific plan to implement to minimise or deal with potential conflict situations in the future.
When things get more complex
If there are sound anti- bullying policies and these are practiced at the workplace and if the workplace bullying is acknowledged and dealt with quickly, then the risk of substantial psychological injury can be minimised.
If the workers compensation claim is assessed in a timely manner and support mechanisms put in place, the psychological damage that has occurred can be treated quickly and strategies put in place to ensure a quick return to work. Even if the injury is significant, a strong support team that includes insurer, worker, and employer and treatment and workplace rehabilitation providers working to together will promote the best opportunity for the worker to recover and return to some form of work.
There are indeed situations where this does happen, and in most cases the best outcomes are achieved in these circumstances. Unfortunately there numerous obstacles that can slow things down, the majority occurring unnecessarily that are the product of an adversarial workers compensations system that it is more concerned minimising liability for some stakeholders than it is with genuine support of bullying victims and putting prevention strategies in place.
What are the obstacles?
1. Slow Claims processing and declined claims
Although there are specific time frames insurers are supposed to adhere to when processing claims and organising assessments and investigations, these can be very lengthy for the bullied worker who is in desperate need of treatment. There are situations where a claim may be legitimate, however sometimes the doctor may make a “technical error” such as not using all the words in a recognised and acceptable diagnosis resulting in the claim being temporarily refused under “reasonable excuse”. This means that the injured worker not only has no access to treatment but also has no income while the decision is being appealed. Although the situation can often be rectified relatively quickly with clarification a change of diagnosis, there are sometimes pressures put on the insurer by the employer to not accept the claim, or a range of administrative and work load issues can mean that it is more than a month before a decision is reached. This can and usually does exacerbate the anxiety/stress the injured worker already has.
2. No suitable duties
Injured workers, whether injured physically or psychologically should not continue to be certified as unfit by their doctor if they have a partial work capacity. This is particularly important when the injury is psychological as there is often a strong fear component in returning to work, particularly to the place where the injury took place. Extended periods of time off work, although initially helpful in reducing the precipitating stressors, can lead to a fear/avoidance and dread of returning to the workplace. The fear can generalise over time into other parts of a persons life where the traumatised persons has felt considerable discomfort outside of work, often when in environments, or places where conflicts could occur. Although it is understandable that the injured worker does not want to experience the distress again under any circumstances, it is important that he/she learns skills to reprocess events, reactions and future behaviours in ways that increases resilience to further distress.
The employer has an essential part in this process. Whereas the psychologist, psychiatrist and doctors treat and manage the symptoms and help the person to develop new coping skills, the employer must provide the environment for these to be practiced. This is likely to mean that initially hours will need to be less than preinjury and the responsibilities and duties at work less and different to pre-injury. In some situations the injured worker may need to be transferred to a different work site. The employer has a legal and ethical responsibility to provide suitable duties if at all possible. When suitable duties are not available the worker’s rehabilitation provider will need to find work, often initially in the form of a work trial with a different employer. This may take some time and can delay the workers recovery and capacity to return to maximum functioning psychologically and with work capacity.
Case Study
John was a 23-year-old trade’s assistant who worked for a successful joinery business in a country town in central west NSW. Unfortunately John is currently off work diagnosed with post-traumatic stress disorder and major depression, the result of two violent assaults by his supervisor over a 12-month period. The first assault was not reported and only came to light after he reported the background and current assault to his doctor when he first sought treatment.
John has worked for his employer for 5 years. He left school at 17 years of age and was hired as a trade assistant. Although John hadn’t become a tradesman he had become a skilled and valuable member of the work team of 15, which serviced 3 or 4 country towns in the area.
Until the most recent assault John liked his job despite the clashes with Rick who was 34 and also happened to be the brother in law and part owner of the business. Rick, according John was a hot head with “real anger issues”, that had become worse in recent years. John believed that a lot of Rick’s uncontrollable rage was the result of increasing steroid use to help him to become more competitive in his body building pursuits.
John reported he was first assaulted by Rick about 15 months earlier. It was not witnessed because he was working off site with his supervisor. According to John, Rick became frustrated and then enraged when he back answered him. He reportedly was grabbed by the throat and thrown against a wall where he hit his head and briefly loss consciousness. According to John, Rick was then remorseful and apologetic and said he would make it up to him. At the time John reported being extremely upset about what happened and felt intimidated and over powered (John is 170cm and weights 79 kilograms. Rick estimates John would be 187cm and about 130 kilograms). Despite what had happened, John reported keeping the matter to himself and not taking it further. He was aware there were no witnesses and it would be his word over his bosses. Also he liked the job didn’t want to lose it. At the time he believed Rick was genuinely sorry and that this was a one off incident.
Over the next 12 months there were more explosive outbursts according to John, though no more violent outbursts - at least that he was aware of or directed at him. Around the time of the second assault and the now current workers compensation claim Rick was reportedly even more on edge than usual. John reported to his psychologist that an incident occurred where he questioned what he was being asked to do. This resulted in Rick grabbing him by the throat, throwing him to ground and strangling him. Another worker was a witness to the incident and intervened to pull Rick off John.
In the following month many things happened medically and legally in relation to the incident. A medical worker’s compensation certificate was issued and a claim lodged with the workers compensation insurer. John’s union was contacted and there were letters of demand and litigation threatened. John’s employer in turn sought legal advice and although offering support to John did not admit liability of the “alleged assault” despite there being a witness who made a statement to the insurance investigator. Rick did not formally acknowledge what had happened and did not apologise as was demanded to apologise by the union and John. He was however required to attend “specialised management training and anger management” however no other disciplinary followed. John did not pursue the matter in terms of attempting to pursue criminal charges with the Police in the first month.
John made a good recovery physically from the choking incident, however, he has struggled psychologically. He was extremely angry and distressed at what had happened. His anger and humiliation was exacerbated further when he read statements about the “alleged assault” (as opposed to “assault”) from his employer and the lack of apology from Rick, believing this was a dismissal from his employer of what had happened and a cover up. Two weeks after the incident, John was enraged to the point of wanting to “takeout Rick by whatever means possible including taking his own life as revenge”. John’s parents who had been his main support were extremely distressed by what was happening and concerned he would suicide.
John’s psychologist was placed in a difficult situation. When John attended the second session of counselling he was accompanied by his father. He was in an extremely agitated state, and made threats of revenge, including discussing how he was going to seek revenge including take his own life at the same time. Over the session some of his anger was diffused, however he was still clearly extremely distressed and traumatised by what happened and admitted if he saw Rick or was in the state of mind he had been in, he could act on his impulses. In following days there were numerous telephone consultations between John’s psychologist, John’s employer, his doctor, the insurer and the local mental health treatment services. His GP was reluctant to “schedule” him against his will for inpatient treatment.
John attended a follow up psychological treatment session 3 days later. Fortunately he was noticeably calmer and it was apparent that he applied some of the strategies and education that had been given about his reactions to managing his distress. The focus of discussion was able to move to the future and working towards other employment options.
Fast forward 2 weeks, a case discussion occurred at John’s doctor’s rooms with John, his father, his psychologist, the workplace rehabilitation provider and a telephone link in with the insurer case manager. John’s distress levels in the previous 2 weeks had continued to reduce and his focus moved towards other types of work with a different employer. John’s psychologist and workplace rehabilitation provider had discussed a number of possible options including working for other employers in his local area. It was agreed by all parties that in view of the circumstances of the “claim”, return to work goals with the same employer was not desirable or achievable and the focus should move towards a different work environment and work team.
John will still need psychological and workplace rehabilitation support in the weeks or months ahead. Although his anger, depression and distress has decreased, his confidence has been shaken, and he easily becomes overwhelmed by anything that reminds him of what happened. John’s psychologist says his psychological assistance will need to encompass self-esteem building, resilience and assertiveness training as well as general encouragement and support. John’s workplace rehabilitation provider will need to continue to liaise with John’s psychologist and GP and identify and screen potential new employers.
3. Psychological Relapse
Good management and support of the psychologically injured worker will minimise the chances psychological relapse occurs. Relapse may occur if the worker is certified as fit for duties before they are ready - i.e. they still exhibit unmanaged symptoms and having limited coping skills, if they are asked to upgrade hours and duties prematurely, if they are exposed to work environments and situations that trigger strong emotional responses that are beyond there coping ability, and when another traumatising or bullying event occurs that is beyond there coping ability, or is contrary to the conditions they were led to believe would occur when they returned to work.
It is important to provide thorough risk assessments of potential situations (hazards) in a workplace that could precipitate relapse. A competent rehabilitation provider will know what to look for, - i.e. support of management, other staff, and a positive organisational culture and will demonstrate excellent communication skills when liaising between stakeholders. When an already injured worker experiences a relapse of symptoms, it can take more time to recover and it may be harder to convince them to attempt to try again.
4. Other issues contributing to cause by following The Psychological Injury
Toxic work places, traumatic events at work and bullying are not the only precipitants of people’s mental health or ill health. A person’s social environment, family support, family background, general health, are just the some of the factors that affect why and how we respond to the demands of life at any given time. With accepted work injury claims there is an assumption that the workers psychological injury was caused at work and it is the main factor why he/ she is now unwell. Other factors however need to be understood by treating practitioners when planning and supporting workers who have been psychologically injured as these factors can influence the nature and extent of symptoms. For example stress and depression that is managed by large quantities of alcohol or other drugs is unlikely to respond as well if little or none of these substances were being consumed. Likewise, lifestyle habits such as diet and exercise, social activity are all “hygiene factors” which need to be understood and promoted when helping the injured worker to recover and maintain their recovery.